This article originally appeared on Focal Points and was republished with permission.
Guest post by Nicolas Hulscher, MPH
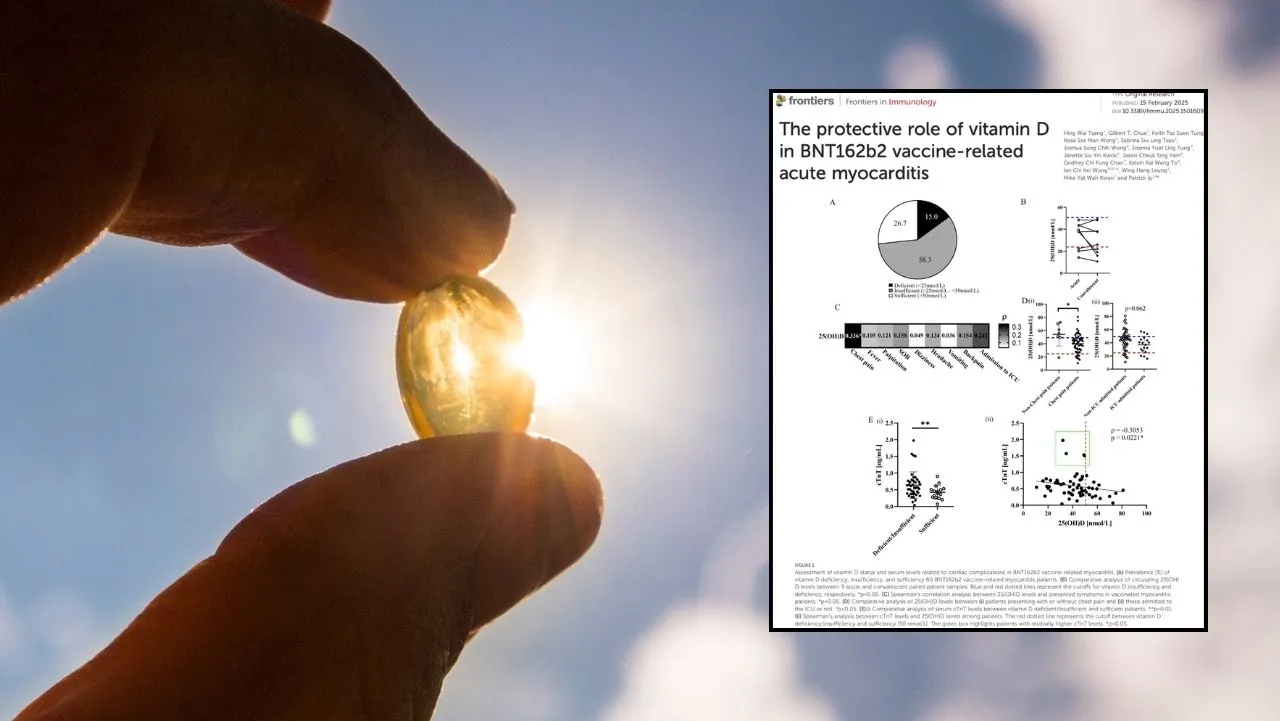
73.3% of myocarditis cases had low vitamin D—linked to higher inflammation, heart damage, and ICU admissions—while sufficient levels were associated with reduced severity.
The study titled, The protective role of vitamin D in BNT162b2 vaccine-related acute myocarditis, was just published in the journal Frontiers in Immunology:
Introduction: Vaccine-related myocarditis is recognized as a rare but important complication, especially after mass-scale mRNA COVID-19 vaccination. Knowledge regarding how to minimize the risk is limited. As NK cells can mediate acute myocarditis after mRNA COVID-19 vaccination and vitamin D may inhibit NK cells via cytokine modulation, we hypothesize that the myocarditis side effect is related to a hypovitaminosis D – mRNA vaccine – hypercytokinemia – NK cell axis, which is amendable to clinical intervention.
Methods: Biochemical, immunophenotypic and genotyping assays were performed to examine vitamin D status and immune profiles in 60 patients who had BNT162b2 vaccine-related acute myocarditis.
Results: A high incidence of hypovitaminosis D (73.3%) was observed in these individuals with vaccine-related myocarditis, particularly in those presented with chest pain or intensive care unit (ICU) admission. Moreover, vitamin D level was negatively associated with peak serum cardiac troponin T level during vaccine-related myocarditis. Genotypically, the GC (vitamin D binding protein) rs4588T allele which encoded the GC2 isoform of vitamin D binding protein was a risk allele, whereas the GC1S isoform was protective. Mechanistically, hypovitaminosis D was associated with higher levels of cytokines pivotal for natural killer (NK) cells (particularly interleukin-1β (IL-1β), IL-12, Interferon-γ (IFN-γ), and IL-8) and higher percentage of CD69+ NK cells in blood, which in turn correlated with chest pain presentation.
Conclusion: These data support the hypothesis that vitamin D plays a crucial role in mitigating mRNA vaccine-related myocarditis by modulating proinflammatory cytokine milieu and subsequent unfavorable NK cell activation, laying a groundwork for preventive and treatment strategies.

Key Findings:
Vitamin D Deficiency is Common in Myocarditis Cases
- 73.3% of individuals who developed myocarditis after mRNA injection had low vitamin D levels (≤50 nmol/L).
- Among those with vitamin D deficiency:
- 88.3% experienced chest pain, compared to those with normal vitamin D levels.
- 30% required ICU admission, indicating more severe cases.
Vitamin D May Reduce Risk
- Higher vitamin D levels were linked to:
- Lower inflammation in the heart (as indicated by lower cytokine levels).
- Reduced activation of NK cells (fewer CD69+ NK cells).
- Fewer severe symptoms of myocarditis (lower cTnT levels and fewer ICU admissions).
- Patients with vitamin D sufficiency (>50 nmol/L) were less likely to experience severe symptoms (p < 0.05).
Lower Vitamin D = More Heart Damage
- Patients with low vitamin D had higher levels of cardiac troponin T (cTnT), a marker of heart damage:
- Vitamin D-deficient patients had an average cTnT of 0.62 ± 0.40 ng/mL.
- Patients with sufficient vitamin D had significantly lower cTnT levels (p = 0.0099).
- Vitamin D levels were negatively correlated with cTnT (r = -0.3053, p = 0.0221).
Click here to read the rest of the article.
Nicolas Hulscher, MPH
Epidemiologist and Foundation Administrator, McCullough Foundation
Please consider following the McCullough Foundation, Dr. Peter McCullough, and Nicolas Hulscher on X (formerly Twitter) for further content.
Copyright 2025 Focal Points